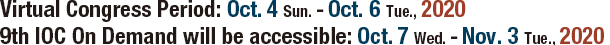
Congress Schedule
A group of sessions will be released at 8:00am and 4:00pm in Japan Standard Time(JST) from October 4 to 6.
Please check what time your local time will be.
As of August 18, 2020
It is subject to change.
| Time | Track #1 |
Track #2 |
Track #3 |
Track #4 |
Track #5 |
Track #6 |
Track #7 |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| All sessions in this time slot will be released at 8 am JST. |
BiomechanicsBiomechanics
Professional Experience and Education
Honors and Awards
Research Interests Biomechanics and orthodontic appliances Abstract Practice of clinical Orthodontics has significantly changed over the last three decades. Our customary work with wires and brackets since last century now includes use of skeletal anchorage devices, orthographic surgery without pre surgical orthodontics and use of sequential plastic aligners to correct malocclusions. However we are still seeking answers to how can we accelerate orthodontic tooth movement to finish treatment sooner. Numerous commercial devices have been promoted, some with spurious claims and others with less than desirable results. Biomechanics
Professional Experience and Education
Honors and Awards
Research Interests Biomechanics Abstract This presentation will deal with biomechanical solutions for maximizing therapeutic efficiency and minimizing side effects during orthodontic treatment. Although various treatment techniques have been developed, it remains quite difficult to predict or compare actual tooth movements subsequent to the application of different treatment mechanics. Therefore, the prediction and planning of orthodontic tooth movement have been largely dependent on clinical experiences. With such a background, the demand for simulating long-term tooth movement under the various treatment mechanics has been increasing to improve therapeutic efficiency and reduce the treatment time. |
The Smile
Education
Professional experience
Recognition
Publication Progressive idiopathic condylar resorption: Three case reports, AJODO 2019, 156:531-544 Research interest Orthognatic surgery Abstract Patients with long anterior face height and anterior open bite often require a surgical approach to correct the vertical dimension. Temporary skeletal anchorage devices now offer the possibility of closing anterior open bite and reducing vertical dimension by intruding posterior teeth. Conversely, patients with reduced anterior facial height (short face syndrome) need elongation of the vertical dimension. In such case, orthognathic surgery is unavoidable if one wants to obtain normal vertical dimension. Review of the literature and case presentation will help to understand the biomechanics and treatment planning of these malocclusion. The Smile
TITLES
DEGREES
Abstract Class II malocclusion is considered one of the most common problems to solve in orthodontics. Differential diagnosis constitutes the main pillar in addressing such deformations in order to be able to apply individualized therapeutic procedures. The Smile
Dr. Chris Chang is the founder of Beethoven Orthodontic Center and Newton's A Inc. in Hsinchu, Taiwan. He received his PhD in Bone Physiology and Certificate in Orthodontics from Indiana University. He is a diplomate of the American Board of Orthodontics and an active member of Angle Society-Midwest. Dr. Chang is the publisher of Journal of Digital Orthodontics and has authored and co-authored many orthodontic books, including Orthodontics Vols. 1-6, as well as Words of Wisdom, Jobsology and Trumpology. He is the inventor of OrthoBoneScrews(OBS). Abstract Maxillary whole arch intrusion and retraction by Temporary Anchorage Devices (TADs) has been proved to be an effective way to improve the esthetics of gummy smile. This lecture will present the diagnosis and treatment planning of gummy smile. Detailed mechanics and screw insertion techniques will be introduced. The rationales for surgical crown lengthening to enhance the anterior esthetics will also be discussed. |
Eruption DisordersEruption Disorders
Honors and Awards
Research interest Bridging Prenatal human development with Postnatal human development Abstract Scientific understanding of the normal eruption process is a prerequisite for an evidence-based prediction and prevention of pathological tooth eruption. Eruption Disorders
Graduated as a dentist from the Dental Faculty in Warsaw, Poland. She finished a postgraduate training in orthodontics at the University in Oslo, Norway in 1997 then worked as a Research Fellow at the Orthodontic Department, Dental Faculty in Oslo until 2002. In 2003 she was awarded a PhD from the University in Oslo for a thesis on autotransplantation of teeth. For the publication from this work she received the American Journal of Orthodontics and Dentofacial Orthopedics Dewel Orthodontic Award in 2002. In 2014 she was awarded a habilitation in medical science from the Medical University in Warsaw on her work related to orthodontic treatment of patients with periodontitis. Dr. Czochrowska was the President of the European Orthodontic Society and she host the EOS Congress in 2014 in Warsaw. She is the President of the Polish Orthodontic Society and the Active Member of the Angle Society of Europe and the European Board of Orthodontists. At present, she serves the position of the Secretary of the Angle Society of Europe. Dr. Czochrowska has organized 2 international congresses on tooth transplantation in 2016 (Sopot, Poland) and 2018 (Rotterdam, the Netherlands). Received Distinguish Teacher Award from the European Orthodontic Society for 2020. At present in the private practice in Warsaw and is working at the Department of Orthodontics, Medical University in Warsaw, Poland. Dr. Czochrowska has authored and coauthored 10 book chapters and 50 scientific articles. She has lectured extensively worldwide on tooth transplantation and orthodontic treatment in patients with periodontal diseases. Abstract Treatment options for impacted teeth are related to the stage of root development, inclination of the impacted tooth, space conditions, status of adjacent teeth and patient's attitudes to treatment. Trans-alveolar transplantation, which is a surgical uprighting of an ectopic tooth, is an attractive option and it is usually performed, when orthodontic extrusion is difficult and extraction of an impacted tooth and orthodontic space closure are unfavorable from orthodontic perspective. Eruption Disorders
Professional Experience and Education
Honors and Awards
Research Interests Orthodontic treatment of impacted teeth Abstract Every orthodontist in the world can align teeth, but when the principle aim of treatment is treating an impacted tooth, it is all or nothing - we either succeed or fail, and it is nothing in-between. Many factors that are not present in routine orthodontics complicate the treatment. The tooth is not visible, therefore accurate diagnosis of its three-dimensional position and relation with adjacent teeth is often difficult. A reliable anchorage unit which allows the application of controlled directional forces with minimal side effects on the anchorage teeth must be build-up. Close cooperation between the orthodontist and the oral surgeon is mandatory for the success of this approach. Mistakes are related to all the aspects of treatment and are not uncommon even in the hands of experts. Failures lead to malpractice lawsuits. However, mistakes sometimes occur due to lack of awareness of the whole dental profession to a specific issue which has not yet been studied and published. This lecture will cover different aspects of treatment of impacted canines and incisors, from what contributes to success through to the reasons for and the circumvention of failure and discuss mistakes seen in hindsight and how to overcome them. |
Early TreatmentEarly Treatment
Dr. Peter Ngan is the Branson-Maddrell Endowed Professor and Chair in the Department of Orthodontics, West Virginia University School of Dentistry. Dr. Ngan is also an Honorary Professor in the Faculty of Dentistry at the University of Hong Kong and a Guest Professor at the Wuhan University School of Stomatology. Dr. Ngan holds a dental degree from Harvard University, School of Dental Medicine and Certificates in Orthodontics, Pediatric Dentistry and Hospital Dentistry from the University of Pennsylvania, School of Dental Medicine/ Children Hospital of Philadelphia. He is a member of the Angle East (Eastern Component of the Edward H. Angle Society). He is a Diplomate of the American Board of Orthodontics and a Diplomate of the American Board of Pediatric Dentistry. He was inducted as Fellow of the American College of Dentists (October, 2008), Fellow of the International College of Dentists (October 2010) and Fellow of the Pierre Fauchard Academy (May 2011). Dr. Ngan's research interest includes growth and development, biology of tooth movement, dentofacial orthopedics, orthodontic appliance therapy, oral implantology, orthodontic bonding systems and adult interdisciplinary treatment. Abstract Young patients with a Class III malocclusion and maxillary deficiency are treated primarily with facemasks. However, because the force is applied to the teeth, the inevitable mesial migration of the dentition can result in anterior crowding and the need for a subsequent extraction therapy. Furthermore, the desired skeletal effect of this commonly used approach often turns out to be less than expected. To increase the advancement of the maxilla, facemask therapy is often combined with rapid palatal expansion (RPE) since stimulation of the midface sutures is expected. Temporary Anchorage Devices (TADs) can be inserted in the palate to avoid mesial migration of the upper molars when using a facemask and to minimize tipping or periodontal damage to the bicuspids /deciduous molars when expanding the maxilla. The author will present early Class III cases treated with the help of TADs and the skeletal and dental changes one will expect with the use of this device. After this lecture, the attendees of this lecture will be able to identify the type of Class III patients suitable to be treated with facemask, RPE and TADs; identify the various factors such as growth pattern, growth potential and the severity of malocclusion that can affect the treatment outcome with this appliance; and learn how to design and fabricate RPE with TADs that can be used in conjunction with a facemask. Early Treatment
Professional Experience Thomas M and Doris Graber Endowed Professor Emeritus, Department of Orthodontics and Pediatric Dentistry, and Research Professor Emeritus, Center for Human Growth and Development, the University of Michigan. Private practice of Orthodontics, Ann Arbor, Michigan. Education Bachelor's degree in Speech, University of California Berkeley; Dental education and Certificate of Orthodontic Specialty, The University of California San Francisco. Master's and Doctorate in Anatomy, The University of Michigan. Honors and Awards Milo Hellman Research Award; American Association of Orthodontists, 1973; E. Sheldon Friel Memorial Award, European Orthodontic Society, 1979; Research Recognition Award, American Association of Oral and Maxillofacial Surgeons, 1983; James E Brophy Distinguished Service Award, the American Association of Orthodontists, Albert H. Ketcham Memorial Award, American Board of Orthodontics, 2008; Beni Solow Memorial Award, European Orthodontic Society, 2011; Edward H. Angle Memorial Lecturer, American Association of Orthodontists, 2014; Angle Heritage Award, Edward H Angle Society of Orthodontists, 2017. Research Interests Skeletal and dentoalveolar effects produced by orthodontic, orthopedic and surgical treatments; normal craniofacial growth and development; the Cervical Vertebral Maturation method of growth assessment. Abstract This presentation describes four decades of research carried out at the University of Michigan that consider the clinical alteration of the transverse dimension of the face, with specific attention given to orthodontic and orthopedic treatment of patients in the early mixed dentition. The results of a series of clinical studies will be described that consider the etiology of dental crowding as well as treatment effects produced by expansion in the early mixed dentition or in the late mixed/early permanent dentition. Early Treatment
Professional Experience and Education Letizia Perillo is full Professor and Dean of the School of Dentistry, Chairman of the NEBEOP Postgraduate Orthodontic Program, Head of the Orthodontic Division at Multidisciplinary Department of Medical-Surgical and Dental Specialties, University of Campania Luigi Vanvitelli, Naples. She is 2018-2020 Visiting Professor at University of Alexandria, Egypt, 2021 Elected President of the Italian Society of Orthodontics (SIDO), 2022 Elected President of the Mediterranean Orthodontic Integration Project (MOIP), 2018-2020 International Ambassador of the American Association of Orthodontists (AAO) for SIDO, Member of the WFO, AAO, EHASO, EOS, SIDO and CH Tweed Foundation (clinical instructor), and member of the Editorial Board of several orthodontic and dental journals. Prof Perillo graduated in Medicine and Surgery in 1986 and specialized in Orthodontics in 1989 at the University of Naples Federico II. She completed her orthodontic training with a postgraduate fellowship at the University of Michigan in 1993 and a PhD in Interceptive Orthodontics at the University of Florence in 1997. Honors
Awards
Research Interests Her main research topics are early treatment, non-extraction treatment, cleft lip and palate, dentofacial orthopedics and genetics. Abstract One of the most heated controversies in Orthodontics concerns the role of early treatment in the correction of dentoskeletal Class II malocclusions by mandibular retrusion. Thus, a treatment for stimulating mandibular growth with functional appliances is often indicated. One of the most famous appliances is the Function Regulator (FR-2), proposed in the 1960s by Frankel. According to the literature, FR-2 treatment is able to correct a Class II malocclusion. However, some studies highlighted an increase in mandibular growth, others reported only restriction of maxillary growth or dentoalveolar effects. This lecture will show primarily the importance of the differential diagnosis in the treatment for dentoskeletal Class II malocclusions, and then the changes associated with the FR-2 treatment and their stability after a 20-year follow-up. |
Interdisciplinary TreatmentInterdisciplinary Treatment
Mithran Goonewardene completed Dental School at The University of Western Australia in 1981 and attended the Forsyth Dental Center/Harvard School of Dental Medicine in Boston, USA from 1984-1987 where he completed his Certificate in Orthodontics and Master of Medical Science degree. He is Head of Orthodontics and Graduate Program Director at The University of Western Australia, is a full member of The Edward Angle Society of Orthodontists and is Certified by the Australian Orthodontic Board. He visits Sri Lanka regularly as a visiting Consultant in Orthodontics in the Dental Institute, Colombo and participates in part-time private practice in Perth. Abstract Interdisciplinary management of complex dental problems may be extremely rewarding for both the treating clinicians and patients. A rigorous systematic approach is necessary to develop a coordinated, patient centred, goal oriented treatment plan. It is critical to establish the needs of the individual patient within their own value system and establish a realistic plan. To achieve the best outcome, clinicians must establish a group of healthcare providers who will bring the necessary skills and knowledge to the interdisciplinary team. They must meet and communicate regularly and effectively through appropriate media. A sequence of activity with specific goals should be outlined, identifying the respective clinicians and their immediate goal, which all clinicians and the patient may refer to at any stage in treatment. The team leader has the responsibility of ensuring that the patient and clinicians are all cognizant of the stage that the patient has reached and what is performed next, in turn facilitating communication. If these processes are adhered to, then the patient and the team can anticipate a mutually rewarding experience with consistently excellent reproducible outcomes. Dr Goonewardene will outline strategies for managing and complex issues related to tooth loss, tooth wear, sleep disordered breathing and complex skeletal problems from an inter-disciplinary perspective. Special emphasis on how to facilitate complex 3 dimensional tooth movements using skeletal anchors will be discussed including application in the surgery first approach. Interdisciplinary Treatment
DDS University of Mainz, Germany Abstract Adults patients affected by severe dentoskeletal malocclusions, multiple missing teeth, and periodontal involvement, require a well-orchestrated interdisciplinary team approach. The primary goal is to provide the restorative specialist with the best possible preconditions for the definitive prosthodontic rehabilitation. Interdisciplinary Treatment
SELECTED AWARDS AND HONORARY DEGREES
Professor Melsen has authored more than 400 publications in the fields of growth based on research of human autopsy material, bone biology and clinical studies. In recent years her interests have focused on the Skeletal Anchorage, Virtual Imaging and Adult Orthodontic Treatment. Abstract While malocclusions can generally be treated by orthodontists alone treatment of degenerated dentitions in adult patients are requiring collaboration of several colleagues, periodontologists and prosthodontists being the most frequently involved. Important is that all aspects of the problem list and the treatment plan is taken into consideration and discussed among the involved dentists and the patient before initiating any treatment. The expectations, the resources regarding time and economy of the patient have to be clear as has the fact that maintenance of the treatment results is required after treatment. The adult patients often demand an aesthetic smile and her/his problem is often far from the main problem. The need and the demand differ. |
APOS Lectures
Education
Professional experiences 1. Faculty of Dentistry, Prince of Songkla University
Research Interest Biomechanics in Orthodontics
2. Thai Association of Orthodontists
3. Digital Dentistry Asssociation
Abstract When Class III non-surgery is planned for the patients, upper and lower incisor positions and inclinations must be decided to indicate types of tooth movement. Subsequently, appropriate biomechanics is established. For the upper incisor, protraction and extrusion are the most often movements while retraction and intrusion are for the lower incisors. Many times, when mandibular rotations are favorable for reducing the concavity of the face, molar extrusion should be introduced. In this presentation, an innovative biomechanics system of upper incisor protraction with extrusion, lower incisor retraction with intrusion, and molar extrusion will be presented. Samples of cases will be introduced in details of clinical applications along with their biomechanics.
Dr. Kook is President of Korean Association of Orthodontists, the Dean of the Graduate School of Clinical Dental Science and the professor of the Orthodontic Department at Seoul St. Mary's Hospital. Currently, he is a Clinical Professor at Department of Orthodontics, Arizona School of Dentistry & Oral Health and Saint Louis Univ. He has published about 100 articles in international peer-reviewed journals regarding corticotomy, arch form, CBCT, and arch form. He also published several book chapters. Diplomate, American Board of Orthodontics Abstract purpose C-palatal appliance(MCPA) is a highly effective device, which can be easily placed and managed by orthodontists.
Professor Johnson Cheng is the Immediate Past President of Taiwan Association of Orthodontists TAO (2017-2018) and the current dean and professor on College of Oral Medicine, Taipei Medical University. He has been the chairman and editor in chief of TAO Journal Committee (2013-2016). He graduated from school of dentistry, Taipei Medical University in 1983 and got Master degree and PhD from the same university in 1995 and 2008, respectively. He practiced in orthodontic department at his hospital and also engaged in teaching and research in his school of dentistry for over 25 years. His major researches were surface treatment of orthodontic TADs and high molecular orthodontic material, esthetic smile in orthodontics, efficient orthodontic treatment of anterior cross-bite, evidence based in orthodontics, etc. He has published over 300 different kinds of academic and clinical papers and been also invited to make lectures about his associated researches around the Asian countries and got an enthusiastic response. Abstract The clinical problems resolution and application of evidence-based information to patients have been much improved since the evidence-based medicine (EBM) developed in two decades. From the history development of EBM, the evidence-based dentistry (EBD) was severely behind than EBM. Most of dentistry remains in the "rule of thumb", representing a lack of scientific evidence, there is a great the improvement of space! For the orthodontics, the relevant discussion of EBD was emphasized only in recent years. This report will be presented first from the development and application of EBD, and then introduce the Cochrane Library website in the Cochrane Database of Systematic Reviews, consists of thousands have been systematic review evidence report on the steps to collect. My meta- analysis and clinical related researches of the smiling esthetic on orthodontic extraction will be described. I will also introduce the clinical application of my evidence-based researches and present lots of interesting clinical orthodontic cases in this report. Finally, I will take some home messages to the audiences about the clinical considerations of smiling esthetics on orthodontic extraction treatment.
Professional Experience and Education
Honors and Awards
Research Interests 3D Technology in Orthodontics Abstract Compromised first permanent molars are relatively common in the adolescent population due to caries and/or developmental defects. Compromised first permanent molars with poor long-term prognosis are commonly associated with both short and long-term clinical dilemmas.
Professional experience and education
Research interest Bone biology Abstract Two female patients presented with gummy smile, maxillary dentoalveolar protrusion and total vertical maxillary excess, retroclined incisors, and increased overbite received orthodontic camouflage with straight wire mechanics by general dentists. The treatments caused severe bowing of upper occlusal plane which aggravated the gummy smile and had led them to seek specialist care. They were successfully managed by orthodontic camouflage and combined surgical orthodontic treatment, respectively, in conjunction with the application of miniscrews on straight wire mechanics. Aggravation of gummy smile by straight wire mechanics, use of visual treatment objective to differentiate between orthodontic camouflage and surgical cases, and LeFort I segmentalization were discussed.
Professional Experience and Education
Honors and Awards
Research Interests Biological background of orthodontic tooth movement Abstract Relapse of malocclusion after orthodontic treatment can be considered as the phenomenon of new malocclusion occurring after active orthodontic treatment due to failure of complete elimination of the cause of malocclusion. Force applied to teeth from the lips, tongue or cheek is thought to be one of the major factors responsible for the relapse of malocclusion. The research that we have been doing suggests that weak continuous forces applied from surrounding soft tissues to teeth possibly play the major role in changes of the position of the teeth. |
Allied Health Professional Program: Clinical Practice and Support Staff(1): Myofunctional Therapy (2): New Digital Technology in orthodontic clinic Clinical Practice and Support Staff (1):Myofunctional Therapy
Professional Experience and Education
Research Interests Diagnosis and Treatment of Dysfunction in Orthodontics Abstract Malocclusion is not merely caused by morphological anomalies and/or improper eruption of teeth, but it is closely related to dysfunctional problems. In addition, diagnosis and training of dysfunctions such as various oral habits etc. are extremely important in executing orthodontic treatment properly. Particularly, in the high degree of difficulty cases, both morphological correction with mechanics and functional training of the patients is quite necessary. Clinical Practice and Support Staff (2): New Digital Technology in orthodontic clinic
Professional Experience and Education
Research Interests 3D analysis of masticatory movement, Straight-Wire technique Abstract Social life has undergone large-scale transformations with the development of digital technology in recent years. These changes are accelerating day by day, with developments in both hardware and software taking place. One advantage of digitalization is the systematic consolidation and organization of large amounts of information, a change that has dramatically enhanced operational efficiency. In the medical field, digitalization has been accompanied by the increased use of keywords such as "3D," "automatization," and "network." The field of orthodontics is currently witnessing a major revolution in diagnosis and treatment as a result of the utilization of digital tools such as CBCT and intraoral scanners. This study explores the effects of digitalization at the levels of research, clinical care, and the operations of clinics respectively, and discusses the future prospects of orthodontic treatment. |
||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Temporary Anchorage DevicesTemporary Anchorage Devices
Professional Experience and Education
Honors and Awards Outstanding Presentation Award, Japanese Orthodontic Society, 2014, 2015, 2017. Research Interests Basis and Clinical Practice of Orthodontic Anchoring Screws Abstract Orthodontic treatment has been advanced by the use of orthodontic anchoring screws (OASs); however, OASs are occasionally loosened during treatment. We then investigated the risk factors for failure of OASs to improve the success rate, and found that the primary stability of OASs is related to the mechanical characteristics of the interface between the OASs and bone in relation to factors such as bone quality and quantity, screw design, placement torque, age, gender and placement site. In this presentation, certain and safety placement techniques for improving the success rate will be discussed in the search for the risk factors for failure. Temporary Anchorage Devices
Professional Experience and Education
Honors and Awards
Research Interests Temporary Anchorage Devices Abstract The Skeletal Anchorage System (SAS) consists of titanium orthodontic anchor plates and monocortical screws that are temporarily implanted in the zygomatic buttress or the mandibular body, or in both, as absolute orthodontic anchorages. The most distinguished feature of SAS is enables us to predictably move molars. The SAS mechanics has revolutionized the concept of orthodontic and orthognathic treatment for adult patients. In this conference, I will focus on Class III patients and discuss how the strategies for Class III correction were changed following the development of SAS. Firstly, it became possible to effectively camoufalge severe Class III maloclusion in adults by distalization of the mandibular molars and/or entire dentition. Secondly, thanks to the development of SAS, it became possible to eliminate or shorten pre-surgical orthodontic treatment and significantly reduce total treatment time in Class III surgical cases. Thirdly, in moderate or severe growing Class III patients, SAS is an extremely effective biomechanics for solving various problems in the second phase treatment. Therefore, the second phase treatment for non-growing patients became more important than the first phase treatment. Thus, nowadays, the SAS becomes an indispensable modality for correction of any Class III malocclusions in my clinical practice. |
Facial EstheticsFacial Esthetics
Dr. Trotman is the Associate Dean for Faculty Development and Professor and Chair of Orthodontics. She received her dental degree from Dundee University, Scotland and her orthodontic degree and MA in Oral Biology from Columbia University, NY. She then completed a Fellowship in Craniofacial Anomalies at the Hospital for Sick Children in Toronto. Subsequently, she was appointed Assistant Professor in the Department of Orthodontics at the University of Michigan School of Dentistry. During her tenure at Michigan, she obtained an MS in Clinical Research Design and Statistical Analysis from the Horace Rackham School of Graduate Studies. Dr. Trotman then was appointed Associate Professor in the Department of Orthodontics at the University of North Carolina (UNC) School of Dentistry. Subsequently, she was promoted to Professor and served as the Interim Associate Dean for Academic Affairs and then Assistant Dean for Graduate Education at UNC. She then was appointed Professor and Associate Dean for Academic and Student Affairs at the University of Maryland School of Dentistry. Dr. Trotman was an American Council on Education Fellow, is a Diplomate of the American Board of Orthodontics, and maintains an active research program funded by NIH with a focus on craniofacial anomalies. Learn more about the Facial Animation Laboratory here. Abstract Patients with facial disability have varying degrees of impaired facial soft tissue movements/function and disfigurement. Surgeons have different treatments that attempt to correct the disability. This presentation will focus on approaches to quantify facial disability and assess treatment outcomes in patients with facial paralysis. Method: Longitudinal 3D changes in facial soft tissue movements were quantified in adults with unilateral facial paralysis (n=36) during different facial animations/movements, and in an age- and sex-frequency matched control group (n=68). Mean group measurements of displacement, velocity and asymmetry of movement were computed. Standard statistical tests were used to test for significant changes over time in the patient group and differences between the patients and controls. Also, 3D dynamic modeling and vector plots (mapping) were computed to isolate patients' abnormal movements compared with the controls. Results: The patients' mean baseline movements were significantly less for both the paralyzed and contralateral sides of the face with much greater movement asymmetry than the controls. Patients' mean measures improved significantly from baseline to 12 weeks, but still fell short of control values. Conclusion: In unilateral facial paralysis, the contralateral facial side was affected by the paralysis and may be tethered or limited in its movement by the paralyzed side. The measures and mapping effectively isolated paralyzed facial regions and tracked patient recovery, and has applications for facial reanimation surgery. A similar approach for diagnosis and outcome assessment will be briefly presented for patients with repaired cleft lip/palate. Facial Esthetics
Dr. Sarver received his DMD from The University of Alabama School of Dentistry and MS in Orthodontics from the University of North Carolina in 1979. He is a Diplomate of the American Board of Orthodontics, a member of the Edward H. Angle Society of Orthodontists, a Fellow in both the International and American Colleges of Dentists and is a Fellow in the American Academy of Esthetic Dentistry. He has had the honor of presenting the Salzmann, Merson and Angle lectures at the AAO Annual meeting. In addition to his private practice, Dr. Sarvers book, Esthetics in Orthodontics and Orthognathic Surgery was published in September 1998. He is also coauthor, with Dr. Proffit and White, of the surgical text Contemporary Treatment of Dentofacial Deformity, and is coauthor the 4th, 5th editions and 6th edition of Proffits classic textbook Contemporary Orthodontics. Publication of his book Dentofacial Esthetics, from Macro to Mini is scheduled to be published in February. He has given more than 400 professional presentations in the United States, Europe, Australia and the Middle and Far East. Abstract The concepts in Macroesthetics to Microesthetics evaluates each patient who walks through your door focusing first on the big picture and then working your way to the minute details in order to treatment plan for the best possible outcome, taking into consideration concepts like esthetic balance and smile projection. Dr Sarver will demonstrate the idea that orthodontics is about more than occlusal function, it is about creating faces and smiles that are functional and beautiful. |
Periodontal ConsiderationsPeriodontal Considerations
Professional Experience and Education
Honors and Awards
Research Interests Craniofacial Growth and Development Abstract Although periodontal implications of orthodontic treatment are well-understood, undesired consequences such as gingival recession, bone dehiscence, and fenestration are still commonly observed. Literature shows that there are anatomic and periodontal boundaries that limit the amount of acceptable tooth movement. In planning orthodontic treatment, it is important to consider periodontal susceptibility, gingival phenotype and morphology of alveolar bone. CBCT imaging is very useful in diagnosing maxillary and mandibular transverse skeletal dimensions, thickness of buccal or lingual bone, and buccolingual inclination of each tooth. Nowadays non-extraction modality has become popular in the treatment of crowded dentition with either traditional bracket systems or clear aligners. However, significant dental arch expansion and incisal proclination often take place, which may result in gingival recession and/or bone dehiscence. Extraction therapy sometimes is necessary to reposition the teeth in the center of the alveolar bone so the periodontal condition can be improved. For certain patients, soft tissue grafting and/or corticotomy in conjunction with bone grafting would be needed. To avoid excessive dental expansion, rapid palatal expansion with TADs can be attempted on young adults to treat narrow maxilla. However, for older adults surgically-assisted rapid palatal expansion or Le Fort 1 osteotomy would be required. In this presentation, the periodontics-orthodontics interdisciplinary treatment approach to maintain the periodontal integrity, minimize future periodontal concerns, and allow efficient orthodontic treatment will be delineated. Periodontal Considerations
Department of Orthodontics and Dentofacial Orthopedics, University of Bern, Switzerland Gingival recession refers to the apical displacement of the gingival margin from the cemento-enamel junction. Recessions can be localized or may involve more teeth or tooth surfaces. Periodontal Considerations
Department of Orthodontics, School of Stomatology, Pek ing University orthodontic treatment is based on the reaction and modeling of periodontal tissue. Therefore, the condition of periodontal tissue is one of the the important factors wich orthodontist must tak e into serious consideration. |
Class II TreatmentClass II Treatment
Professional Experience and Education
Honors and Awards
Research Interests Dentofacial Orthopedics Abstract This lecture will illustrate patient-related factors that potentially can improve the efficacy of Class II treatment. Two such factors will be discussed: 1) timing of treatment, defined on the basis of reliable indicators of individual skeletal maturity, and 2) individual patient responsiveness. Class II Treatment
ABBREVIATED BIOGRAPHICAL SKETCH Dr. Joseph Ghafari earned dental degrees from the Université Saint Joseph (Lebanon) and the University of Pennsylvania (U/PA, USA), and orthodontic education at Harvard University/Forsyth Dental Center. He is a former Professor and presently Adjunct Professor of Orthodontics at U/PA. He is Professor and Founding Head of the Division of Orthodontics and Dentofacial Orthopedics, American University of Beirut. A Diplomate of the American Board of Orthodontics, and past or present President of national and international associations, he has a rich portfolio of research, publications, and invited lectures worldwide. He has received awards and recognitions from various professional organizations and academic institutions. EXTENDED BIOGRAPHICAL SKETCH Dr. Ghafari earned dental degrees from the Université Saint Joseph, Beirut, Lebanon, and the University of Pennsylvania School of Dental Medicine, and orthodontic education at the Harvard School of Dental Medicine/Forsyth Dental Center. He rose to the rank of Professor at the University of Pennsylvania. He is Professor and Founding Head of the Division of Orthodontics and Dentofacial Orthopedics at the American University of Beirut and Adjunct Professor of Orthodontics at the University of Pennsylvania. He also founded the postgraduate orthodontic program at the Lebanese University dental school. Among a rich array of research projects, Dr. Ghafari was the Principal Investigator of a prospective clinical trial supported by the National Institute of Dental and Craniofacial Research, in which alternative approaches are compared in the early treatment of Class II, Division 1 malocclusion. This field remains a centerpiece of his research activities, expanding into component analysis of this and other malocclusions (notably Class III), the development of which was linked to functional problems in childhood. The outcomes of these investigations relate to diagnosis, timing and assessment of treatment, and the recognition of various phenotypes within the same malocclusion type that respond differently to treatment. In all the above tracks, Dr. Ghafari has promoted interdisciplinary and interprofessional research, namely with basic medical sciences, engineering, public health, nutrition, and psychology. Most of Dr. Ghafari’s numerous (over 100) publications report primary research data in American and international journals and books chapters; he is also the co-author of the book Orthodontics at Crossroads. Dr. Ghafari is the proponent and former Editor of Short Communications of the American Journal of Orthodontics and Dentofacial Orthopedics. He is a member of the Editorial Board of the Journal of the American Dental Association, the Editorial Director of this journal’s Middle East Edition, and on the Editorial Board of Seminars in Orthodontics. Dr. Ghafari is a Diplomate of the American Board of Orthodontics and a member of many national and international associations, including the American Association of Orthodontists, The Edward H. Angle Society of Orthodontists (Eastern Component), and fellowship in the American and International Colleges of Dentists. He served as President of the Craniofacial Biology Group of the International Association for Dental Research, President of the Greater Philadelphia Society of Orthodontists, President of the Harvard Society for the Advancement of Orthodontics, and he is the founding President of the Lebanese section of the IADR, the Lebanon Association for Dentofacial Research. Dr. Ghafari received academic and professional recognitions from various organizations and institutions, including an honorary MA degree and the Earl Banks Hoyt Award from the University of Pennsylvania, the Vincent De Angelis Award from the Harvard Society for the Advancement of Orthodontics, and the Brainerd F. Swain Award of Excellence from the Edward Angle Society, Eastern Component. ABSTRACT “Personalized” rather than “generic” treatment of Class II, Division 1 requires consideration because of various constitutional and therapeutic limitations. Because of variable genetic and environmental components of individual malocclusion related to dentoskeletal and/or soft tissue profile, some Class II phenotypes may not be transferred through treatment to a Class I phenotype. |
Edgewise Appliance
Edgewise Appliance
Professional Experience and Education
Honors and Awards
Research Interests Evidence-based orthodontics. Materials science. Esthetics. Abstract INTRODUCTION : Self-ligating brackets are still being actively promoted by their respective distributors. What are the advantages to use these brackets in light of the existing literature ? |
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
| All sessions in this time slot will be released at 4 pm JST. |
WFO Keynote Lecture
Professional education
Academic Appointment
Academic Activity
Award
Abstract Irregularities of the teeth and unacceptable facial appearance have been human concerns since the Greek and Roman periods. The word “orthodontics” was first used in a book published in the late 18th century by Pierre Fauchard. Norman Kingsley published a book entitled “Treatise of oral deformities as a branch of mechanical surgery” in 1880 in which he introduced the mechanics of tooth movement and its biological tissue reaction. More recently, Edward Angle had a great influence on modern orthodontics. While orthodontic clinical treatment has been built on these and other forefathers, patient care in 2020 and beyond demands more than historical precedent. Currently the terms “evidence-based orthodontics” and “evidence-based treatment” are often used in orthodontic clinical and research publications to validate a particular therapeutic approach. What is the actual “evidence” for what we do as orthodontists and where does it come from? Development of knowledge in the areas of molecular biology, craniofacial growth and development, histological tissue reaction, dental materials, as well as the improved use of statistics have supported the current theoretical basis for orthodontic treatment. As a result, there has been increased development of technical procedures for patient care. Looking to the future, we need to focus on individual patient variables by better monitoring differences in the biological and psycho-social backgrounds among patients. Future clinicians considering orthodontic treatment planning will need to cultivate an “individualized diagnostic eye,” based on improved understanding of more broadly based and identified patient characteristics. |